Opioid Strategy Overview
Drawing on a public health framework, TennCare’s opioid strategy centers around primary, secondary, and tertiary prevention of opioid addiction.
- Primary prevention: seeks to reduce the risk of TennCare members progressing to opioid addiction or dependence. This level of prevention centers around TennCare members who are new or non-chronic users of opioids.
- Secondary prevention: seeks to reduce the impact of opioid use for TennCare members by engaging in early detection and intervention. This level of prevention centers around TennCare members who are women of childbearing age, as well as of TennCare providers.
- Tertiary prevention: seeks to provide evidence-based addiction recovery supports for TennCare members with opioid dependence or misuse.

As noted, a significant component of TennCare’s opioid strategy involves establishing a high-quality Substance Use Disorder (SUD) and Opioid Use Disorder (OUD) treatment network for members. To accomplish this, TennCare focused on four key milestones:
- Establishing a Medications for Opioid Use Disorder (MOUD) program description and quality standards;
- Building access to and capacity for a high-quality provider network across the care spectrum;
- Increasing the coordination of care and clinical integration; and
- Identifying opportunities for value-based interventions within a high-quality OUD and SUD treatment network.

Coverage of Opioids
TennCare contracts with a Pharmacy Benefit Manager (PBM) to administer the TennCare pharmacy benefit. As part of the contract agreement with the PBM and at the direction of TennCare, the PBM implements and operationalizes point-of-sale (POS) edits at the time a prescription is processed at the pharmacy. The process of implementing new POS edits has been iterative over the years to ensure the best outcomes for our members and has focused on opioid prescriptions for many years. TennCare now has a coverage benefit limit in place for opioids.
Effective January 16, 2018, TennCare and its PBM implemented a point-of-sale (POS) edit on agents in the Short-Acting and Long-Acting Narcotics classes of the Preferred Drug List (PDL). For first time or non-chronic opioid users, TennCare will cover opioid prescriptions for up to 15 days in a 180-day period at a maximum dosage of 60 morphine milligram equivalents per day (MME per day). After the first-fill prescription (less than or equal to 5 days), a member can receive up to an additional 10 days of opioid treatment with prior authorization (PA). Some clinical exceptions (e.g. patients with sickle cell, new diagnosis of cancer, hospice) exist to these POS edits through prior authorization. The goal of this policy change is to reduce overexposure to opioids both in dosage and duration for first-time and acute opioid users. The medical evidence strongly shows that increased duration both in dosage and in length of exposure greatly increases the risk of long-term chronic opioid use and other potential negative health outcomes associated with chronic opioid use and misuse. By reducing the coverage of opioids for first-time and nonchronic users, TennCare’s goal is to reduce the number of members who progress to becoming chronic opioid users over time.
As of 2017, TennCare no longer covers a prescription for a patient receiving a short-acting or long-acting opioid with a cumulative daily MME greater than 200 MME. This recommendation was a part of the CDC chronic pain guidelines. The goal of this policy is to slowly reduce the dosage among chronic users to reduce the potential for overdose or diversion.
Prior Authorization (PA) requirements and POS edits also help to mitigate the risks of improper usage of opioids. The following requirements are in place to mitigate the risks of improper use of opioids/ controlled substances:
- All long-acting opioid agonist medications require prior authorization.
- After the first-fill prescription (less than or equal to 5 days), a member can receive up to an additional 10 days of opioid treatment at a maximum dose of 60 MME per day in each 180-day period with prior authorization.
- All controlled substances have associated measures that mitigate risk of improper use including POS edits, quantity limits, prospective Drug Utilization Review edits and prior authorization requirements that discourage unsuitable use, Prescription Monitoring Program (PMP) checks, and appropriate monitoring.
The length of time the PA remained active before needing to be renewed for short-acting opioid agonist medications was also reduced from 6 months to 3 months in 2016. The goal of this policy change was to prevent abuse and overutilization of the opioid agonist prescription.
TennCare has also changed the Preferred Drug List (PDL) over time to prevent misuse of opioids and other controlled substances. The changes to the PDL include shifting agents with high-risk of misuse potential to non-preferred status as well as applying monthly quantity limits first to individual agents and later on a cumulative basis.
For example, in 2014 TennCare started only approving non-preferred short-acting opioid agonist medications if a patient could not use any preferred agents due to a contraindication, drug to drug interaction, or history of toxic side effects that cause immediate or long-term damage with all preferred agents. More recently, TennCare is attempting to prevent exposure to high dosages of opioids by limiting benefit covered days of supply and daily morphine milligram equivalents (MME) for non-chronic or new users of opioids.
Non-Pharmacological Pain Management and Clinical Services
Chiropractic services are covered for both TennCare members under the age of 21 and aged 21 and older.
Managed Care Strategies for Proactive Engagement of Women of Childbearing Age
TennCare has partnered with the Managed Care Organizations (MCOs) and the Pharmacy Benefits Manager (PBM) to use data analytics to identify potential clinical risk for women of childbearing age using opioids. This model uses risk stratification to identify members into different severity categories which include risk groupings such as those at high risk for developing opioid addiction or opioid use disorder. The MCOs use information from the model to provide appropriate forms of member engagement, outreach and possible intervention.
TennCare continues to decrease barriers to voluntary Long-Acting Reversible Contraception (vLARCs) for members. In 2016, the MCOs worked effectively with TennCare to make vLARCs more readily available at the time of delivery to meet members where they are. Reimbursement of immediate postpartum vLARCs was unbundled from the global obstetric billing to facilitate rapid access to all forms of contraception rather than waiting until a follow-up visit to place the vLARC.
For more information please contact the Managed Care Organization directly:
Wellpoint |
BlueCare |
UnitedHealthcare |
| For referrals related to women of child bearing age, please contact Provider Services: 833-731-2149 Referrals can also be sent to: WLPBehavioralHealthRef@wellpoint.com |
Cheri Moreland, VP, Member Engagement and Systems Innovation Cheri_Moreland@bcbst.com |
Tammy Thompson, RN, CCM Clinical Manager 952-406-5974 TammyThompson@uhc.com |
In 2021, TennCare partnered with Stellar Pharmacy, to implement an inventory management program using their proprietary smart dispensing cabinet called XpeDose™. The XpeDose™ cabinet is placed in the provider’s office/clinic stocked with a full array of vLARCs and replenished as needed free of charge. XpeDose™ software facilitates claims processing in real time and dispensing of a vLARC at the point of care. XpeDose™ technology greatly improves TennCare's ability to sustain operational controls and program oversight to ensure members' ongoing same-day access to intrauterine and implantable contraceptive device options.
For more information on Xpedose™, call Stellar at (629) 335-4400 or email vLARCatTennCare@xpedose.com.
Treatment of Individuals with Opioid Use Disorder
TennCare covers a variety of treatment options for individuals with opioid use disorder including withdrawal management and medications for opioid use disorder at inpatient, residential, and outpatient levels for substance use disorder and opioid use disorder.
Buprenorphine Enhanced Supportive Medication Assisted Recovery and Treatment (BESMART) Program
BESMART was developed in 2018 to be a specialized provider network developed by each Managed Care Organization focused on contracting with high quality medications for opioid use disorder (MOUD) providers to provide comprehensive care to TennCare members with opioid use disorder (OUD).
Since its implementation in 2018, TennCare’s opioid strategy has demonstrated a significant impact on both members and providers.
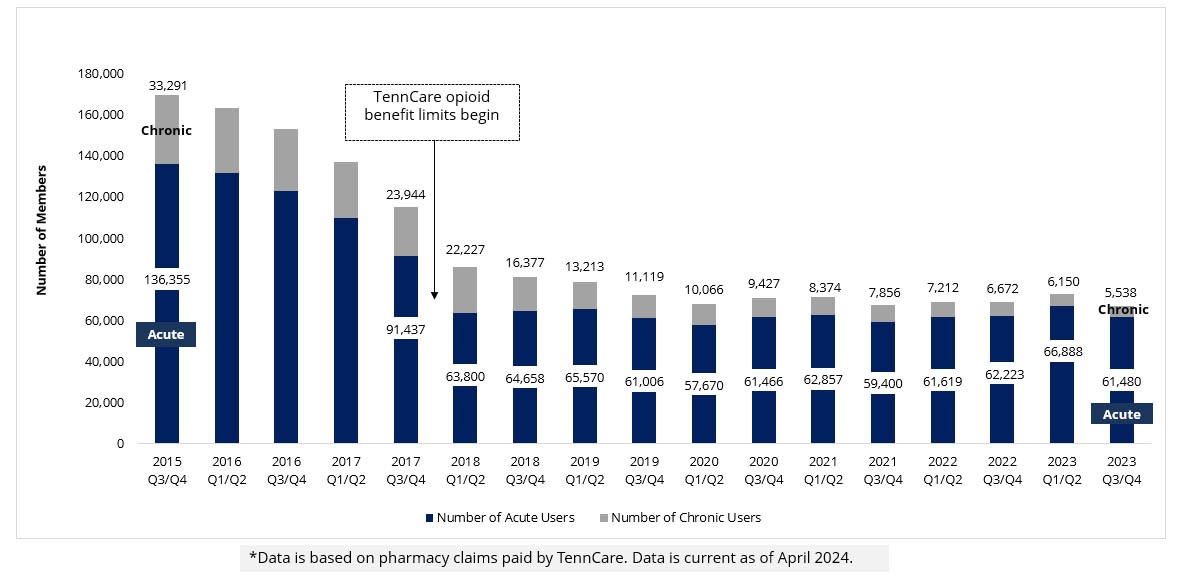
TennCare Acute and Chronic Opioid Users
Overall, the number of TennCare new, acute opioid users has declined by 55% since 2015. The largest decrease occurred following the implementation of new TennCare opioid benefit limits.
TennCare Prescription Patterns for Acute Opioid Use
81% of all first time and acute opioid users are now receiving 6 days or less of opioids after new limits implemented. This reduction in the days of supply for opioids for members decreases the likelihood for developing addiction.

Neonatal Abstinence Syndrome
The rate of neonatal abstinence syndrome (also known as neonatal opioid withdrawal syndrome) births among TennCare recipients has decreased for several successive years and remained stable over the past three years. Further information is available in the annual NAS report.
